A quick story about biometric testing and wellness screening: My neighbor asked me to look at his car that was spewing white smoke. He asked, “Do you know what the problem is?” You don’t have to be a mechanic to know that white smoke coming out of a car is a really bad thing.
It is a symptom of a much larger problem, in this case, a cracked engine block. Radiator fluid getting into the engine causes the white smoke. This problem is fatal, and the only solution is a complete engine rebuild.

He was asked, “Did you notice the car acting funny?” He replied “No, but a long time ago the check engine light came on.” He got tired of seeing the warning every day, so he covered it with black electrical tape, making it easier to ignore.
Had he taken his car to a mechanic, he would probably still have a functioning car today. The check engine light was an early warning signal that something was not quite right.
We all have early warning signals that come from our body when something is not quite right. We don’t get check engine lights. Instead, we get indications of high blood pressure, high blood glucose, and high blood cholesterol.
The biometric testing measures that come from our body can act as early warning signals that something is not quite right. If we ignore them, just like my neighbor ignored his check engine light, the odds of developing potentially fatal chronic diseases go way up. Biometric testing, or wellness screening, is a foundational aspect of every successful wellness program.
It allows individuals to identify early warning signals. Among US adults, there are a lot of early warning signals coming from high blood pressure, high blood cholesterol and high blood glucose. Government-sponsored surveys found that about 80% of all wellness programs included biometric testing. This chart shows the types of screenings included.
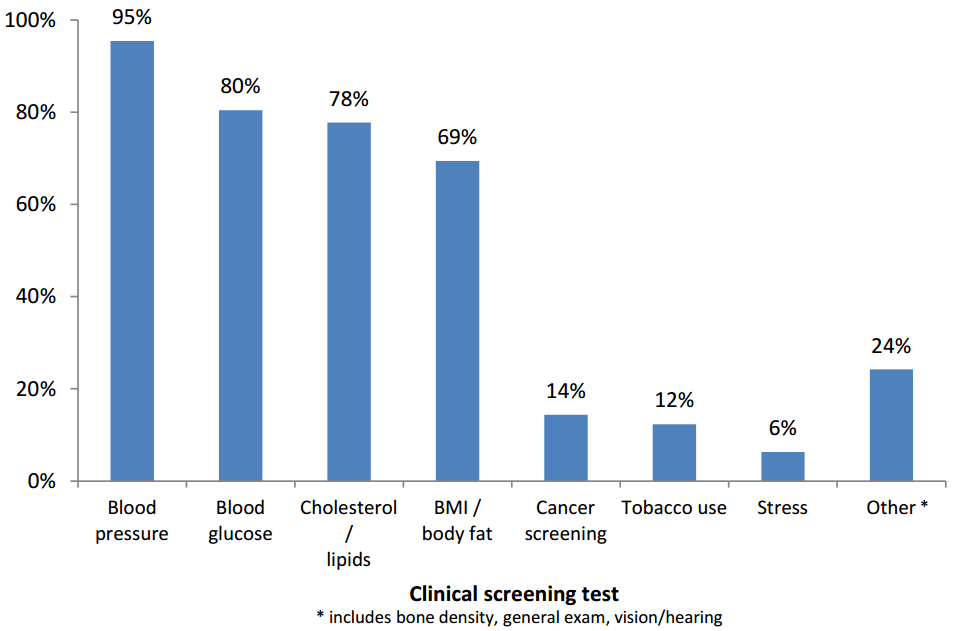
The number one thing workplace wellness screening programs are testing for is blood pressure, followed by blood glucose, blood lipids, and body mass index or body fat. These four risk factors are the main focus of almost all screening programs.
Increased competition and increased availability of screeners has made the cost of screening relatively low. It doesn’t take much to take a quick look at each of these four risk factors.
Why Do Biometric Testing or Wellness Screening?
In the past 100 years, large epidemiological studies have shown us that elevated health risks are associated with the prevalence and incidence of major chronic diseases. All of these studies point to a very strong association between high levels of blood pressure, blood cholesterol, blood glucose, and body fat and chronic diseases such as heart disease, cancer, and diabetes.
These connections between elevated health risks and chronic disease are strong. During this same time frame, we have learned that if you can lower elevated health risks, chronic disease incidence also declines. As Americans have worked to lower elevated health risks, the prevalence and incidence of heart disease has dropped substantially. Today heart disease death rates are lower than they have been in nearly 75 years.
The most recent data shows that for every 100 adults, 53 have elevated blood cholesterol, 33 have elevated blood pressure, and about 10 are type 2 diabetic. Most adults in the United States have at least one elevated health risk and around half of them don’t know it. Finding people with elevated health risks and helping them adopt and maintain healthy behaviors is the key to lowering chronic disease prevalence and early death.
Wellness programs that can help individuals identify their health risks and improve their health behaviors will have a direct impact on the length and quality of life of their employees. Wellness screening and intensive follow-up are probably the single most important thing wellness programs can do to improve employee health.
Despite the health advantages of having lower health risks, there is another reason why employers offer biometric screenings. Many employees like to track their own personal health. Biometric testing is like your own personal health dashboard.
Your own personal biometric data is a snapshot of your health. Elevated health risks can be predictors of future health and low health risks can be indicators of ideal health. For many people, there is something inherently pleasurable in seeing low risk scores. Contrary to national recommendations, some people like to get their biometric values every year just because they can.
How to Do Biometric Testing?
There are many options when it comes to gathering biometric data. If many of your employees are located in one geographical location, you might consider using onsite wellness screening companies where a vendor comes in and gathers biometric data for all your employees at once.
If you have remote employees, multiple locations, or logistically cannot perform onsite screenings, your options include at-home testing kits, individual screenings with a primary care physician, or individual appointments at a third-party screening facility. On-site wellness testing can cost between $45 and $70 but may require a minimum number of individuals.
Getting biometric data during a physician’s office visit generally costs between $100 and $200. It’s cheaper for groups that are self-insured to do screening on site but if your organization is fully insured, employees can get their biometric data measured for free as part of their preventative services (which are now covered by most health plans). Take-home biometric testing kits cost between $40 and $50 each.
Besides the cost of the actual testing, there are other costs that employers need to know about. Encouraging employees to do a biometric testing will cause some employees to have a physician’s visit and possibly start taking medications. That office visit and those new medications are additional costs that can add up.
I am currently analyzing the pharmaceutical costs for a wellness program. Early evaluations suggest that employees who do wellness screenings have higher pharmaceutical costs than those who do not. This is expected because medication is the most common medical treatment for elevated health risks. Biometric screening prevents chronic diseases and early death, but workplaces should understand that all preventive services come with associated costs.
There are many good options to get screening work done. The bigger challenge is to organize and track the screening data you collect. WellSteps has experience helping employer groups do this in a variety of different ways. On-site screeners can generally provide an Excel file of all biometric data since WellSteps is a third-party vendor.
Individual employees who get their biometric data from a kit or their personal physician can email or fax a copy of their results. One of the quickest and easiest ways for wellness programs to receive wellness screening results from individual employees is to use the WellSteps app.

Employees open the app, take a picture of their wellness screening form, and the system automatically uploads it to a secure file. The WellSteps staff then verifies that the information is complete and uploads the biometric values so that it integrates with personal health assessment data. Just about everyone has a smart phone, which means just about everyone has a way to quickly and easily verify that they’ve completed their wellness screening.
Most of the time, individual employees who participate in WellSteps will upload their data from a recent physician’s visit. Over the years, WellSteps has used a variety of partners to conduct wellness screenings.
Acquisitions and mergers within the industry have influenced both the price and quality of the screenings. WellSteps currently uses Onsite Health Diagnostics, but we are always reevaluating our vendors to make sure we have the best in the industry.
How Often Should Employees Do Wellness Screening?
There are two ways to answer this question. They both depend upon the goals, objectives, and budget of your wellness program. The most effective and cost-effective way to screen employees is to follow the professional guidelines that have been written by the U.S. Preventative Services Task Force.
These guidelines are not perfect, so they will and do change–but at the moment, they are the best we have. The Preventive Services Task Force provides guidelines that specify when screening is appropriate, based on age, gender, and risk factors. It is NOT recommended to screen an entire employee population every year.
Relative to other wellness interventions, screening is quite costly. The cost of annually screening every employee is always greater than any possible savings that might come from reduced chronic disease incidence or premature death. This approach makes the economics of mass biometric testing very dubious.
For example, if you screen for a risk that is present in 10 out of 100 people, you have to screen all 100 people just to find that 10 individuals who have elevated risk. Then you have to help these 10 at-risk individuals adopt and maintain healthy lifestyles for the rest of their lives. And, if all goes well, some of these 10 people will avoid chronic diseases they would have otherwise developed.
The table recommends wellness screening intervals for blood pressure, glucose, and cholesterol. The Task Force reviews hundreds of research studies and provides these current recommendations to balance screening costs with reducing chronic disease incidence and prevalence.
Risk Factor
Wellness Screening Interval
Hypertension
The optimal interval for screening adults for hypertension is not known. The Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) recommends:
● Screening every 2 years with BP <120/80.
● Screening every year with SBP of 120-139 mmHg or DBP of 80-90 mmHg
Diabetes (glucose)
The first step should be measurement of blood pressure (BP). Adults with treated or untreated BP >135/80 mm Hg should be screened for diabetes. The optimal screening interval is not known. The ADA, on the basis of expert opinion, recommends an interval of every 3 years.
Hypercholesterolemia
The optimal interval for screening is uncertain. Reasonable options include every 5 years, shorter intervals for people who have lipid levels close to those warranting therapy, and longer intervals for those not at increased risk who have had repeatedly normal lipid levels.
An age at which to stop screening has not been established. Screening may be appropriate in older people who have never been screened; repeated screening is less important in older people because lipid levels are less likely to increase after age 65 years.
Most workplaces either don’t know about these recommendations or they don’t care. That is unfortunate, because they represent an enormous amount of careful research, consideration, and recommendations by an independent panel of professionals! The recommendations are the best information we have on how often to conduct wellness screenings.
Despite these recommendations, some clients have insisted that WellSteps screen their employees every year. They ignored the scientific guidelines because their employees liked to track their own biometric testing data. A pretty expensive way to monitor data that doesn’t change much over time.
Not long ago, I worked with the CEO of a large construction company. He was excited to show me his biometric scores for each of the last 15 years. His cholesterol levels, glucose levels, and blood pressures had fluctuated a little bit each year but were essentially straight horizontal trend lines across the entire 15-year period. He was proud of the fact that little had changed in 15 years, even though one of his risk factors was borderline high during that entire time.
The fact that he had not worsened was good news, but the point is that some people just like to view their own data. Unfortunately, some of these people are decision-makers, who think everyone should be as data-driven as they are. They believe that tracking and monitoring data will change behavior, though this is not the case.
Armed with the U.S. Preventive Service screening recommendations, I consulted with a group to help them see that doing biometric testing every year was not a smart use of time and money. We calculated the potential savings and discussed the specific recommendations. But then we talked about how much the employees loved getting their biometric data each year.
Employees mentally associated the screening with a monthly reduction in their healthcare insurance premium because it had been part of their incentive plan for many years. Each year, all the employees who wanted the healthcare premium reduction had to complete the biometric testing and each year, many of the employees were excited to share the results with fellow employees. The act of screening itself had become part of the workplace culture.
Despite the potential cost savings from following the recommendations, they continued with annual testing. They valued the screening process more than the savings associated with following national recommendations. Annual screening had become a ritual within this organization that everyone looked forward to and actually enjoyed.
After hearing their arguments, it became clear that the second answer to the question, “How often should employees get screened?” was as often as you like. This particular group has been doing annual wellness screening for over five years and to them, the extra cost of the screening was worth it.
So, there are really two answers to the “how often” question: 1) follow established screening science so you can optimize your wellness dollars OR 2) throw the science to the wind and let your employees engage in an annual biometric screening ritual so long as you have the budget for it. And neither one would be wrong.
Biometric Testing and Wellness Screening is Easy – It’s What Comes Next That Matters
Despite what actually happens in many wellness programs, there are actually two important parts of having a successful biometric testing program. The first part is gathering data (bloodwork and measurements) and generating risk scores. This is the easy part. In fact, it’s so easy you can buy a kit and do it yourself at home.
The medical professionals or vendors are trained to take your blood and calculate your results. The hard part is knowing what to do with the information once you have it.
Lowering elevated blood pressure, glucose, or cholesterol–now that is a different issue altogether. At the end of the day, isn’t that the reason for the screening in the first place? This whole situation reminds me of a Seinfeld sketch. You know, the one where Jerry talks about the difference between taking a car reservation and actually holding the reservation.
Typically, an employee who has recently received their biometric data will visit with a nurse or a health coach. They will discuss the results and make recommendations. It is likely they will give the employee a brochure with encouragement to visit a primary care provider.
This is all well and good, but this is also where the process breaks down. They will strongly encourage employees with dramatically elevated health risks to seek medical attention. The proper medical treatment protocol for elevated cholesterol and blood pressure is to first start with Therapeutic Lifestyle Change (TLC).
This is a fancy way of saying adopting and maintaining a healthy lifestyle. This is the correct approach to take with elevated health risks. Because, after all, the elevated health risks are almost always just a symptom of a larger problem: unhealthy behaviors.
If individual employees with elevated health risks adopt and maintain habits that include good nutrition and regular physical activity, meaningful improvements in their health risks will occur. Despite this treatment protocol, most physicians are only able to provide some encouraging conversation and perhaps another brochure.
There are very few options to engage in therapeutic lifestyle change within the current medical community. Doctors are not reimbursed to have conversations with their patients. They get paid when they put something in you or to take something out of you. Many doctors don’t ever talk about healthy lifestyles with their patients because they don’t believe patients will do anything anyway.
Why waste time talking about good nutrition and physical activity if the patient is unlikely to make the necessary behavior changes? Often, they are quick to prescribe risk reducing medications. These medications work, but they don’t address the underlying problem of unhealthy behaviors.
To help employees with elevated health risks, wellness programs need to offer effective programming. This means programming that is based on effective behavior change concepts. These can be challenges, campaigns, courses, or coaching. Any and all of these are designed to help employees and their significant others improve nutrition habits and exercise patterns.
WellSteps does this by offering specific behavior change campaigns, challenges, and WellSteps TLC. This program is effective at reducing elevated cholesterol, blood pressure, blood glucose, and body fat found during a wellness screening without medication. If employees have high health risks after multiple attempts and considerable efforts to adopt healthy behaviors, then it’s time to start taking risk reducing medications.
[video_embed URL=”https://vimeo.com/337630577″]
Headwinds
Even with effective programming, it is hard for most people to lower their health risks. Besides the usual suspects–fast food, large serving sizes, processed foods, and sugar–there are other factors. These factors are actively working against employees who have elevated health risks. On average, as you age each year, wellness screening blood pressure, cholesterol, and glucose values increase.
After age 30 cholesterol values increase. In females they increase about 3 mg/ml per year and in males about 1 mg/ml per year. After age 30, males and females will experience a blood pressure increase of about 1 mm/HG every year. Blood glucose does the same thing. After age 30, most adults will experience an increase in blood glucose of about 1 mg/ml per year.
This means that with the passage of time, employees who were once low risk will eventually become high risk. It also means that individuals who are high risk will get even higher. In ten years’ time, many healthy employees will have acquired elevated health risks.
For most people, these risks are elevated because of unhealthy lifestyles. The elevated risks are a result of a physical reaction to unhealthy behaviors. Genetic causes of elevated blood pressure are very real. But they are not as strong as behavioral factors. Genetic causes of high blood cholesterol are extremely rare, less than 1 percent.
There is, however, a natural flow of risk. Or, as the academics like to call it, natural risk migration that occurs each year. The complicated figure below shows how this works. Among a typical group of employees there will be some who have low risk, some who have moderate risk, and some who have high risk.
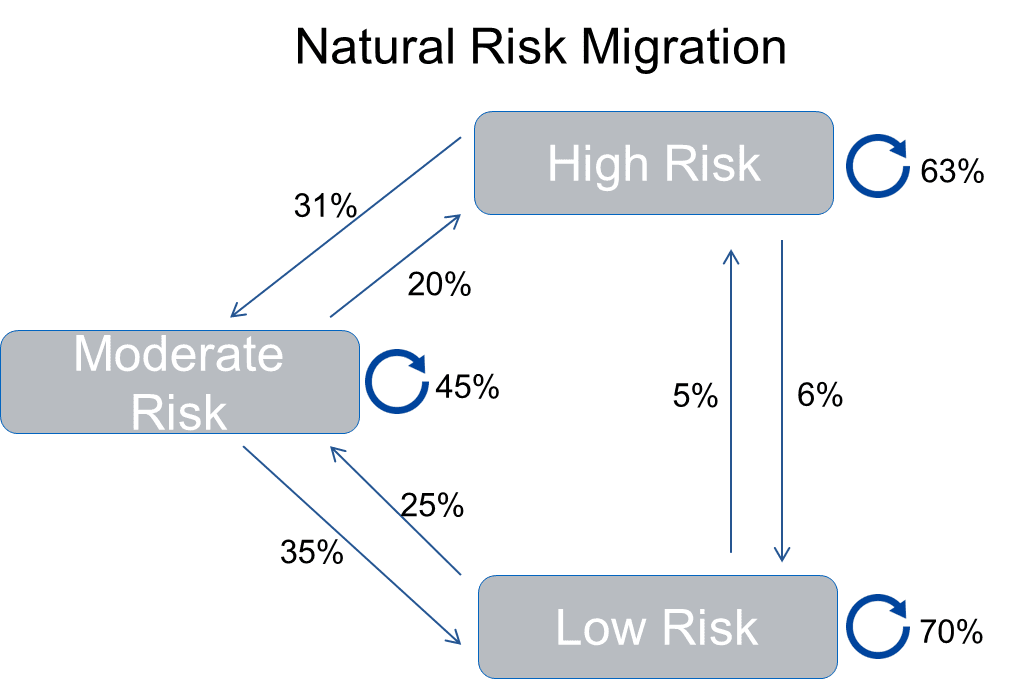
In just one year, many employees will move from one group to the other. Take for example, the employees who are low risk at the beginning of the year. In 12 months, 70% of those employees will still be in the low risk category. However, 5% will migrate from low risk to high risk. Another 25% will migrate from low risk to moderate risk.
Even though they did not participate in any wellness programs or any intervention whatsoever, there will be a natural flow between risk levels. Most employees who have moderate risk at baseline stay there. But, 20% move to high risk and 35% become low risk. In the high risk group, most of them stay high risk after 12 months. An just 6% move to the low risk group and another 31% move to moderate risk.
This is the natural risk migration that occurs with most adults. This movement reflects changes in health risks that occur naturally.
Every wellness program must consider the natural risk migration that occurs among their employees. To document that a wellness program is having any effect on elevated health risks, your risk migration needs to be better than the natural risk migration that occurs.
With natural risk migration, it is possible that 6% of your high risk population may have become low risk even though your program didn’t do anything. Be careful not to claim credit for changing employee health risks when similar changes can occur naturally. Researchers, myself included, spend a lot of time looking at the impact of wellness programs.
We are extremely careful to document that our programs do indeed change risk. And they change risk in ways that are significantly greater than natural risk migration.
Biometric Data Security
When personal health information is collected, all HIPAA privacy, security, and breach rules must be followed. Privacy policies on collection, storage, and disclosure must be provided and a third party must be used to analyze data. If you have questions on the compliance of your wellness program, use the free compliance checker tool here.
Putting It All Together
Biometric testing (wellness screening) and subsequent behavior change are some of the most rewarding aspects of employee wellness programs. This is where we save and transform lives. We have fun and do fun activities, but at the end of the day, it’s about improving the length and quality of people’s lives.
An effective wellness program that is focused on behavior change can make a big difference in health risks. Good wellness programs save lives. I’ve spent most of my adult life documenting the effects of wellness programs. I would have to say that helping people reduce their health risks is one of the more rewarding things I have ever done. Here is the typical process we take to help employees lower their health risks:
Get the Word Out
We have used the Know Your Numbers campaign to communicate, educate and motivate employees to get screened. We use the best marketing and messaging possible to persuade people that getting screened is a good idea. It works best when the employer group includes a meaningful incentive. Once everyone has been screened and their biometric data has been integrated with their personal health record, employees can see what risks they have.

Include Everyone in Your Wellness Screening
One approach to helping employees change behaviors is to focus only on those employees who have elevated health risks. This is a pretty good strategy to take because you’re focusing on the worst cases first. However, natural risk migration tells us that with the passage of time most people will eventually develop elevated health risks.
You can focus on those employees who have elevated health risks and help them improve behaviors, or you can take a step back and consider offering behavior change interventions to every employee including those with low health risks. This makes sense for several reasons.
As people age, their health risks will increase and eventually more and more of your employees will develop elevated health risks. Also, by offering behavior change campaigns to all your employees at the same time, you can capitalize on the group effect. The group effect happens when a large group of employees are simultaneously engaged in a single cause.
To help people lower blood cholesterol, they should eat more vegetables. Getting the entire workforce to participate in the Veggie Up campaign means that all the employees are improving their vegetable consumption at the same time.
There’s always a sense of competition, camaraderie, and peer pressure that helps individuals have more success as a group than as individuals. WellSteps prefers to include all employees in behavior change campaigns and challenges, regardless of their health risks.
Again, targeting those with health risks is not a bad strategy but we have found that including everyone in the adoption and maintenance of healthy behaviors has a more comprehensive and lasting impact.
Using this exact approach we have published a variety of research studies documenting changes in employee health risks. The table below shows the changes in biometric health risks over a one year period among the 3500 employees of Boise School District. To get employees to participate, they were offered a $40 a month reduction in their health insurance premium.
These results are typical of what we’ve seen for large groups of employees participating in a variety of behavior change campaigns. The results are favorable, but still not as good as when we use TLC. Here is the full paper that describes this program in more detail.
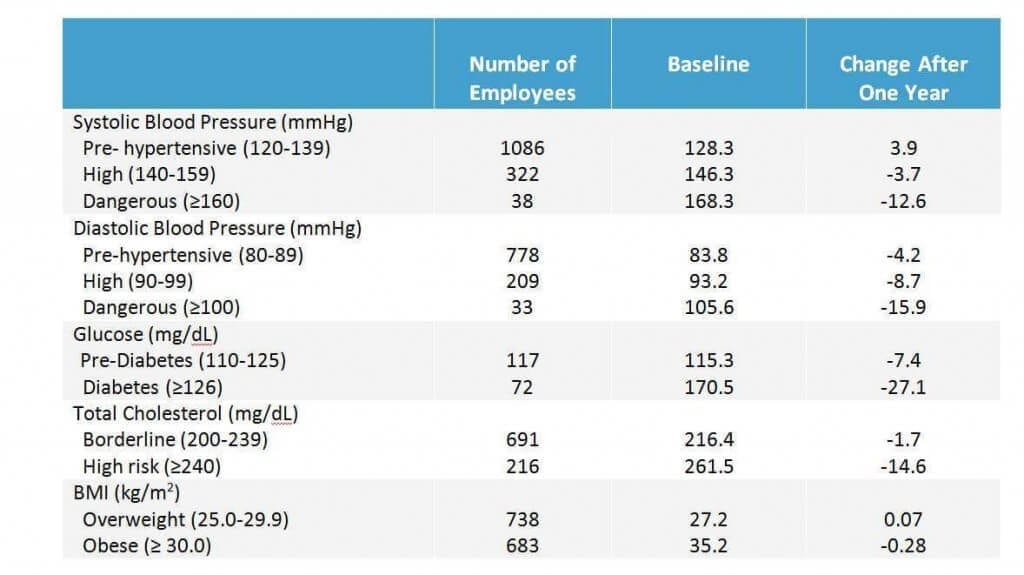
Boise School District is not the only workplace that has been able to produce results like this. Over the years I have published many studies that show that aggressive behavior change programs, both in the community and in workplaces, can reduce elevated health risks in as little as six weeks. Even better results are seen at 6, 12, and 18 months.
I am not the only one who’s been studying the impact of wellness programs and wellness screening on elevated health risks. Every year the Koop Award is given out to the best wellness programs in the United States. Almost without exception, every one of these programs has been able to demonstrate dramatic improvements in health risks.
Bring Out the Big Guns
The hardest thing for people to do is to change behaviors. Elevated blood cholesterol, blood pressure, and blood glucose doesn’t just happen overnight. These elevated health risks developed over decades of exposure to unhealthy lifestyles. Since it takes decades to develop these elevated health risks and the habits that precede them, reversing the process can be difficult.
For some employees, participation in some targeted behavior change campaigns and challenges will make a difference, but for others a more aggressive approach is required. This is why WellSteps has developed WellSteps TLC. WellSteps TLC is a Therapeutic Lifestyle Change program that consists of extensive behavior change programming that specifically targets employee nutrition and physical activity.
It includes all of the education, tools and strategies, motivation, and support from others that individuals need to successfully adopt healthy behaviors. It is a clinically backed program that teaches and encourages changes in nutrition and physical activity that result in lower employee health risks.
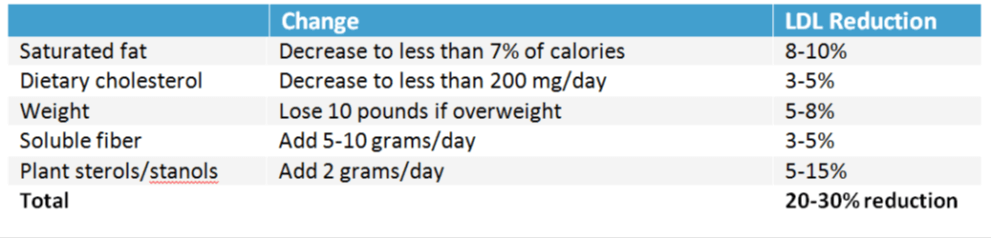
For example, employees with elevated blood cholesterol benefit greatly from TLC. Employees who will decrease their saturated fat to less than 7% of total calories can reduce their LDL-cholesterol by 10%. Here’s what the research shows about the impact of TLC.
Each TLC module includes video, behavior change tasks, social support, and gamification. Participants can participate via computer or using any mobile device. Each module is interactive and participants must complete simple behavior change tasks before they can progress to the next module.
Each time employees participate, they can interact with others who are working through the same lifestyle transformation. The program includes healthy recipes, cooking and food shopping ideas, and discussions from behavior change experts.
After participating in TLC, if an individual still has elevated health risks, it’s time for employees and their spouses to work with their healthcare provider to get more aggressive with risk reducing medications. Medications are effective at reducing elevated health risks and they have the ability to reduce the prevalence of chronic diseases.
So What is Next For Your Company’s Wellness Screening Options?
If the goal of your wellness program is to improve employee health and reduce healthcare costs, then helping your employees complete a wellness screening and behavior change program are a must. Done right, biometric testing and subsequent behavior change programming will likely be the most effective part of your wellness efforts.
Any wellness program that can document significant reductions in elevated health risks is well on its way to reaching its wellness goals. Improved health risks is also a good indicator that the wellness program has been properly designed and executed. Schedule a free demo with WellSteps and discover how you can design your wellness program today!
Frequently Asked Questions
What do they do at a wellness screening?
Wellness screenings (or biometric testing) involves either a fingerstick blood draw or a venipuncture. A qualified health provider will also collect data such as blood pressure, height, weight, and waist circumference.
How long does a wellness screening take?
The screening typically takes about 10-15 minutes.
Why are wellness screenings important?
By knowing your numbers, you can detect health problems early. As you get older, you can monitor these numbers and make necessary lifestyle changes.
Wellness Screening Participant Experience
“My wife encouraged me to get a wellness screening, since I am 31 and have never done one before. I finally listened to her and got a blood draw with my doctor. It was shocking to find out that I have Hashimoto’s, just like my wife! Now, I have started taking levothyroxine and I feel so much better. Without checking my biometrics, I would never have known about this disease. It was worth it!”
